Stroke based community resources
Apps and online resources for stroke patients
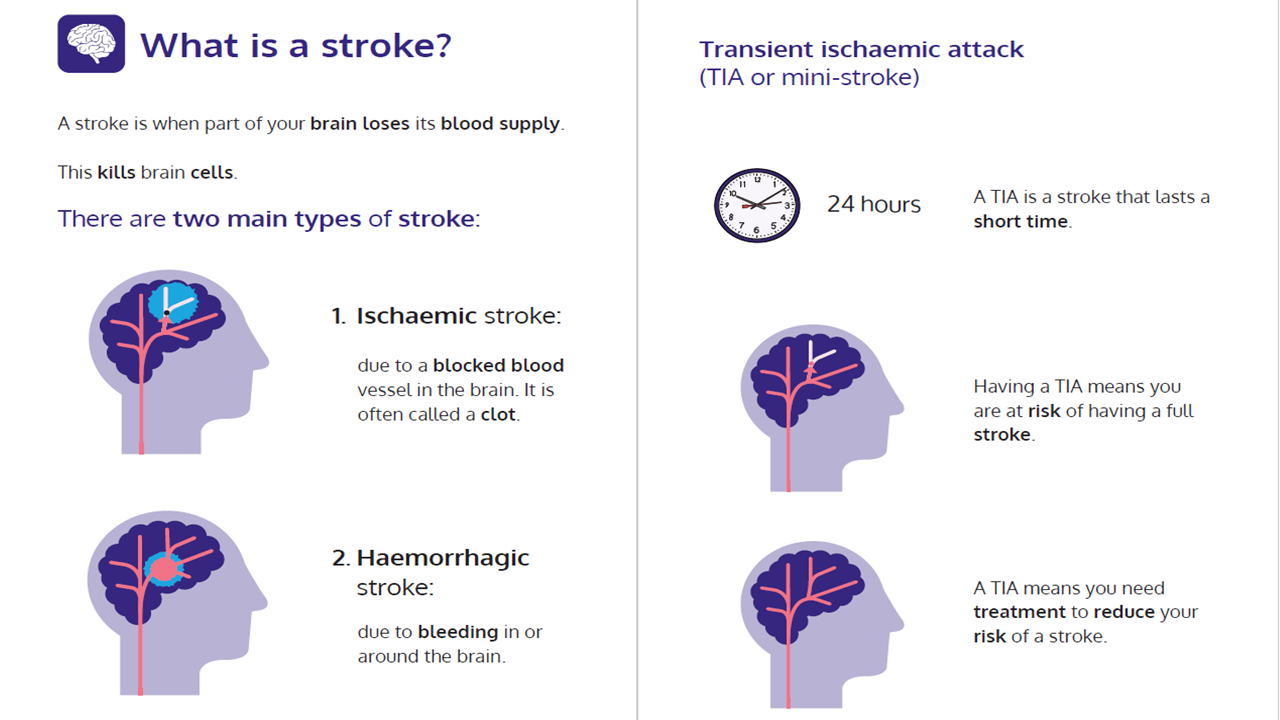
What is a stroke?
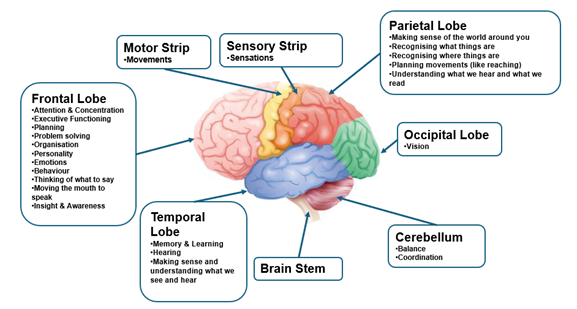
The brain has a cortex which is the thinking part of the brain (it is wrinkly and composed of grey matter).
It is divided into two hemispheres – the left and the right.
The left side of the brain controls the right side of the body, and vice versa.
It is important to know that sometimes people do not have difficulties which visibly affect the left or right sided of the body.
The brain carries messages between its different parts via cells called neurons.
There are billions of neurons which form complex pathways and networks, which transport the messages within the brain.
The brain also carries messages backwards and forwards to the body via the brain stem and spinal cord.
Like all organs, the brain needs oxygen and nutrients transported by the blood to function properly. If the supply of blood is restricted or stopped, brain cells begin to die.
Areas of the brain that can be affected:
Why is rehabilitation important?
After a stroke, damaged areas in the brain cannot re-heal themselves.
Over time, however, the brain can form new pathways in attempts to regain the skills and functions affected by the stroke. The ability of the brain to continually change and adapt is known as neuroplasticity.
Rehabilitation encourages the brain to start making new connections which helps you to recover. One of the most effective ways to promote neuroplasticity is through exercise and task practice, this why you will be asked to complete tasks outside of therapy sessions.
Secondary prevention
Many strokes are preventable. Different factors can increase your risk of stroke, including:
- Smoking
- Drinking
- High Cholesterol
- High blood pressure
- Atrial fibrillation
- Inactivity
- Being overweight
- Diabetes
There are various methods for managing these factors, including through changes in your diet, keeping hydrated and ensuring you take your medications as prescribed.
You can manage your blood pressure and cholesterol by staying active, limiting your salt intake, maintaining a healthy weight, avoiding or managing stress, avoiding excessive alcohol use and quitting smoking.
The Stroke Association have a page dedicated to managing your risk of further stroke. Please follow the link below for more information.
https://www.stroke.org.uk/stroke/manage-risk
Stroke Association
The Stroke Association is a charity that offers insight into the effects of a stroke and the recovery. They organise support groups and online activities and advise on what services could help you in your area. They also provide support to the carers and families of stroke survivors.
For further information please see the Stroke Association website:https://www.stroke.org.uk/ or contact their helpline on 0303 3033 100
Exercises
There are several different resources available to help you with your recovery. The exercise resources include online videos, apps, face to face groups or individual sessions. These are outlined below. We have also added some general exercise sheets that you may find useful.
Exercise videos
Different Strokes
Different Strokes provide a range of online videos set at 5 different levels of ability ranging from no active movement (carer assisted) to fully independent.
Each level has a programme of 12 sessions which focus on varying key elements, such as:
- Mobility and movement
- Cardio
- Strength
- Core and Flexibility
https://differentstrokes.co.uk/online-exercise-for-stroke/
Stroke Association in partnership with A Stroke of Luck
They have jointly produced stroke-specific online exercise videos with 3 different levels:
A Red Group is for people with limited mobility.
An Amber group for those with some mobility.
A Green Group for people who are independently mobile.
They have different videos for strengthening different parts of your body, stretching, coordination and relaxation.
https://www.stroke.org.uk/blog/stroke-specific-exercise-video-programme
Community stroke groups (including exercise)
Walton-on-Thames Stroke Group: https://waltonstrokegroup.co.uk/
Email chairman@waltonstrokegroup.co.uk / 01932 247549
Woking Strokeability https://wokingstrokeability.com/index.html
Email secretary@wokingstrokeability.com / 01483 323575
Arm related exercises
Exercise sheets
If your physiotherapist has advised you are safe to do exercises independently, you can try some of the exercises in ‘independent arm exercise’ document attached below. It’s good to be aware that a stroke affects everyone differently and you may find some of these exercises too challenging or you may not be able to move your arm as shown in the picture. If this is the case, you can either focus on the exercises you can complete or try activating your muscles statically.
Click here for independent arm and hand exercises
If you are unable to complete the exercises independently, have a look at these links for ‘Assisted Exercises’ here or alternative exercise here.
Repeat each of the exercises until your muscles feel tired or your technique worsens. If you are concerned your technique is not correct, do not continue with the exercise and consult your physiotherapist or occupational therapist.
Graded repetitive Arm Supplementary Program (GRASP)
GRASP is an arm and hand exercise program for people with stroke. It can be undertaken by the patient on their own. It is highly recommended that it is completed with assistance from caregivers or family members. They advise a minimal movement criterion of some wrist and shoulder movement.
They offer the program, manual and GRASP books free of charge.
Visit their website for more information: https://neurorehab.med.ubc.ca/grasp
If your physiotherapist has advised you are safe to do exercises in lying or sitting independently, you can try some of the exercises for ‘independent’ exercise. It’s good to be aware that a stroke affects everyone differently and you may find some of these exercises too challenging or you may not be able to move your leg as shown in the picture. If this is the case, you can either focus on the exercises you can complete or try activating your muscles statically.
If you are unable to complete the exercises independently, have a look at the ‘Assisted Exercises’. Repeat each until your muscles feel tired or your technique worsens. If you are concerned your technique is not correct, do not continue with the exercise and consult your physiotherapist.
Click this link for independent leg exercises
Click this link for assisted leg exercises
Gym referrals and sports
Your GP, physiotherapist or occupational therapist can refer you on your local ‘Exercise/ Gym referral schemes’. Following this, you will have an assessment with a physical activity specialist to determine what programme of physical activity fits your specific needs. After this assessment you will have an opportunity to engage with a physical activity programme, at a discounted rate.
Sports-based groups
There are several charities and groups that support you to engage with sport and physical activity. There are also often exercise and social groups run at your local day centre. You can learn more about the day centres in your area by contacting your local council or searching on https://www.connecttosupportsurrey.org.uk/
Sport in Mind
Sport in Mind uses sport and physical activity to improve the lives of people experiencing mental health problems, from those who have severe difficulties to those who do not have a formal diagnosis.
They hold weekly drop-in sessions at various locations in Surrey.
Sessions vary from Tai Chi, and yoga to badminton, table tennis and football.
Visit https://www.sportinmind.org/surrey for more information and their current timetables.
Disabled Golf Association
The Disabled Golf Association is a charity supporting people with disabilities to access golf events and improve their wellbeing.
Events take place around the country from March to October at various golf courses. People can go along informally or enter the competition if you have an official handicap.
They also offer taster sessions for people who wish to learn how to play golf.
Visit for https://disabledgolf.org.uk/ more information.
Woking Wheels for All
Wheels for All offers all-ability cycling using its fleet of adapted bikes: trikes, quads, recumbent, side by side and standard 2 wheelers.
Sessions are based at the athletics track at Woking Sportsbox.
Visit https://wheelsforall.org.uk/locations/woking-wheels-for-all for further details.
Apps for exercise
There are also several apps that can help guide you through exercise videos and progressions. Some are available at a cost and others are free of charge. Find out more here.
Arm recovery
Following a stroke, your arm may be weaker, tighter or you may find it hard to control the movement. You may also struggle to feel it or sense when it is being touched. Below, we have provided a more detailed overview of why you experience these various symptoms and how you can manage or improve them.
Arm Weakness
A stroke can damage parts of the brain that control signals to the muscles. This can cause them to get weaker because you are not able to use them. With time, they gradually become more deconditioned and weaker. Doing exercises aims to improve strength in your muscles and help your brain to recover the parts of it that control your muscles.
We have provided an overview of some exercises that could support your recovery.
If your occupational therapist or physiotherapist has advised that you need support when you are completing exercises, try some of the exercises outlined in the ‘assisted exercises’ link. Ensure you seek help of a family member or carer. Your helper will need to adjust the level of support they give you depending on how much you can do.
If you can complete exercises without support, please review the independent exercise link.
Queen Square upper limb programme
Queen Square offer an intensive 3-week upper limb programme that focuses on individualised goals relating to functional tasks.
For an individual to be referred, they must have some forward reach and at least the beginning of thumb and/or finger extension. They also need to be able to participate in goal directed training and tolerate a 3-week intensive programme. Therefore, some people who have very stiff and painful shoulders and/or problematic spasticity in the wrist and fingers need local review before being considered for the programme.
If you believe you fit the criteria to be referred, please discuss this with your GP, physiotherapist or occupational therapist.
Spasticity
A stroke can damage part of the brain that control signals to the muscles. This can result in an increase or decrease in muscle stiffness. When the muscle stiffness is increased, it is known as increased ‘tone’. Increases in tone can make it harder to stretch and move. For example, as you walk, you might find your arm gradually starts to bend. This is likely the result of increased tone.
It is likely that you will have been assessed for these changes while you were in hospital. Your physiotherapist or occupational therapist might have given you exercises, stretches and a splint to manage the changes in ‘tone’ and maintain the range in your joints. It is important you follow the advice previously given as these changes often require long term management.
If you have been given a splint, you should use the splints as prescribed by your therapist. If you notice any discolouration or marks on your skin, you should contact your GP or your therapist.
Sometimes, when tone is not managed effectively, it can lead to long term changes in muscle length and movement. For example, you may find it difficult to wash your hand because you are unable to straighten your fingers to get to your palm.
If you have difficulty managing the changes in your tone, you should seek further advice and support from your physiotherapist, occupational therapist or GP.
Splints
As a result of tightness or increased tone you may be required to wear a splint to help stretch your arm/hand when you are resting.
If you have been given a splint or orthotic for your arm, you should use the splints as prescribed by your therapist. If you notice any discolouration or marks on your skin, you should contact your GP or your therapist.
If your splint is wearing out, broken or not fitting well please ask your GP to refer you for review/replacement as below:
‘Off the shelf’ splints are provided and managed by the surgical appliance department at Ashford and St Peter's Hospitals NHS Foundation Trust
If you have a ‘custom made’ splint you will need to be reviewed by the hand therapy department Ashford and St Peter's
If there are changes to your needs affecting your function it may be useful to also ask for a review with an occupational therapist at this time.
Leg Recovery
Following a stroke, your leg may be weaker, tighter or you may find it hard to control the movement. You may also struggle to feel it or sense when it is touching the ground. Below, we have provided a more detailed overview of why you may experience these symptoms and how you can manage or improve them.
Leg Weakness
A stroke can damage parts of the brain that control signals to the muscles. This can cause them to get weaker because you are not able to use them. With time, they gradually become more deconditioned and weaker. Doing exercises aims to improve strength in your muscles and help your brain to recover the parts of it that control your muscles.
We have provided an overview of some exercises that could support your recovery.
If your occupational therapist or physiotherapist has advised that you need support when you are completing exercises, try some of the exercises outlined in the ‘assisted exercises’ link. Ensure you seek help of a family member or carer. Your helper will need to adjust the level of support they give you depending on how much you can do.
Lower limb spasticity
See our section on spasticity on this link
Splints/Orthosis
As a result of weakness or increased tone you may be required to wear an orthotic to support the position of your leg when walking or a splint to help stretch your leg when you are resting.
If you have been given a splint or orthotic for your leg, you should use the splints as prescribed by your therapist. If you notice any discolouration or marks on your skin, you should contact your GP or your therapist.
Splints and orthotics are provided by surgical appliances at Ashford and St Peter's Hospitals NHS Foundation Trust.
If your splint is wearing out, broken or not fitting well please ask your GP to refer you to the surgical appliances at Ashford and St Peter's Hospitals.
If there are changes to your needs affecting your mobility it may be useful to also ask for a review with a neurophysiotherapist.
Learn more about sensory changes in the section below:
Sensory changes
After a stroke, your sensation can be affected. The pathways from the brain to areas of the body are complicated and sensory problems are different for everyone.
The changes in sensation may mean you:
- Are unable to feel someone touching your arm or leg,
- You experience more pain when there isn’t a true cause for this. For example, you may have pain when your arm or leg is touching sheets on your bed
- You may not notice whether something is hot or cold in temperature, or it may be harder to tell the difference
- You may also find it difficult to know the position your body is in
- You may not be able to recognise objects in your hand.
You may also experience tingling, prickling, numbness, aching, burning or pins and needles.
Change or lack of sensation can make the hand and foot vulnerable to damage.
Therefore, to reduce this risk, it is important to:
- Change positions frequently to prevent too much pressure on the affected limb or areas
- Always make sure your hand or leg is in a safe position and not stuck underneath anything or hanging down
- Be conscious of applying more force than necessary when gripping objects
- Observe your skin for damage regularly
- Keep skin soft and hydrated by washing and massaging it.
- Be aware of scalding or burning and take care with hot water, radiators, sitting too close to a fire
To prevent burns:
- Check the temp of water with the unaffected hand first
- Wear silicon gloves while cooking
- Use insulated mugs for hot drinks
Treatment
Treatment for sensory changes includes sensory re-learning. This means attempting to retrain or stimulate sensory pathways. Techniques include:
- Touching different textured objects
- Touch discrimination exercises such as touching or holding objects of different sizes, shapes, and weights
- Tactile object recognition. This means trying to distinguish what object is in or touching your hand. For example, trying to recognise whether you are holding a pen or pencil.
- Massage
- Vibration e.g. using a vibrating massage ball over the affected limb
- Exercises that reflect daily activities e.g. placing your hand on the kitchen work top while you make a cup of tea or resting your hand on the toothpaste tube while you brush your teeth
- Temperature discrimination exercises
- Joint position exercises. For example, replicating the position of your unaffected arm or leg on the affected leg and vice versa.
Evidence suggests you should do 60 minutes a day 3 times a week.
Communication and swallowing
Communication

A speech and language therapist (SLT) can help you to improve your speech, reading and writing as much as possible.
We can also help you to learn other ways to communicate. These are known as compensation or coping strategies. They include anything from gestures to electronic devices - anything that can help you get across what you want to say.

Speech and language therapy isn't just about the time you spend with your therapist. Your communication will only improve with practice, so the work you put in outside of your therapy sessions is just as important.
What kind of communication problems do people have?

Aphasia affects your ability to speak and understand what others say. It can also affect your ability to read and write. Aphasia is a common problem after stroke and around a third of stroke survivors have it. It will affect people in different ways.
Please see this leaflet about communication after stroke created by the Stroke Association Your communication after a stroke: Aphasia friendly leaflet.
Aphasia Therapy Online: This is a free website to practice listening, spelling, reading and naming. Available in 9 different languages with multiple options for increasing/decreasing difficulty: https://www.aphasiatherapyonline.com/
Word finding difficulties

Some people experience word finding difficulties following a stroke. This leaflet outlines what word finding difficulties are and some strategies to help - Word finding leaflet.
Here is an aphasia friendly version of our word finding leaflet - Aphasia friendly leaflet.
Dysarthria

Dysarthria is a difficulty controlling the muscles in your face, mouth and throat usually due to weakness, making it difficult to speak clearly. This can mean that your speech becomes slurred or slow or that your voice sounds quiet. This leaflet outlines some strategies that may help - Clear speech strategies.
Here are some exercises that may help to make your speech clearer - Clear speech exercise pack
Apraxia of Speech

Apraxia of speech is when you have difficulty moving the muscles in your face, mouth or throat in the order you need to when you're speaking (co-ordination difficulty). This can make it difficult for other people to understand you. This leaflet explains what Apraxia is in more detail - What is Apraxia of speech.
Additional information leaflets on Apraxia:
- Apraxia of speech strategies
- Apraxia of speech advice for carers
- General strategies for communication partners following a stroke
Communication groups and other support
Below is some information on local services who may be able to support you.
Please click on this link to print or download the list of services available.
Swallowing

SLT offer support with swallowing difficulties by providing dietary advice, referral for instrumental assessment of swallowing and if appropriate exercises may be provided.
Please see below leaflet on swallowing difficulties after stroke created by the Stroke Association.
https://www.stroke.org.uk/sites/default/files/Dealing_with_swallowing_problems.pdf
Safe Feeding Techniques
We have produced this short video, which has been endorsed by the Royal College of Speech and Language Therapists, designed for healthcare professionals and anyone involved with feeding patients with eating or drinking difficulties. Find out more on this link.
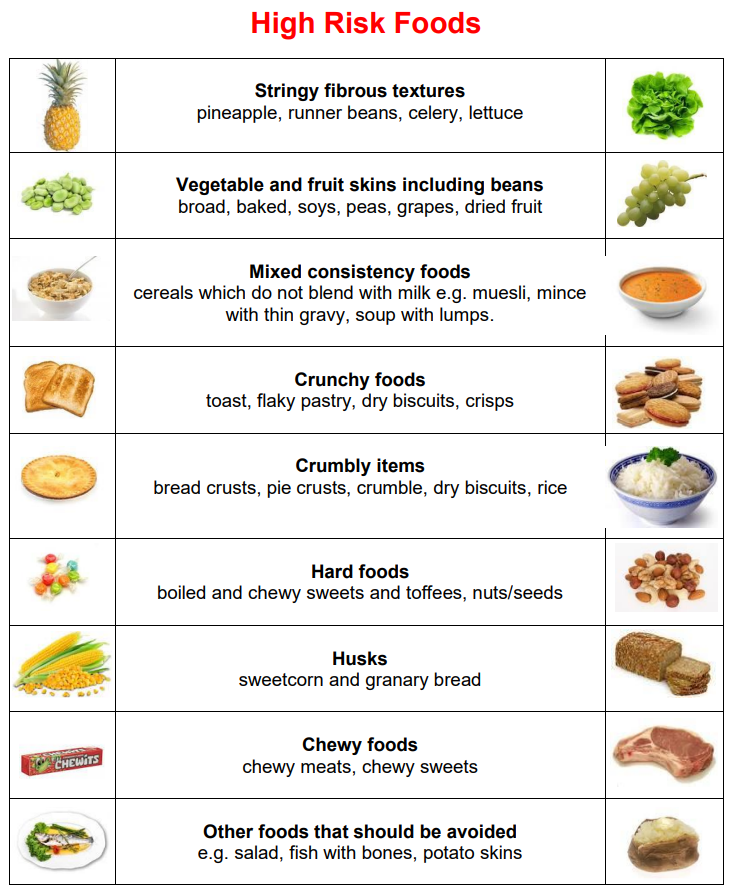
High risk foods
A SLT may recommend that you take a normal diet but avoid or take more care with certain high-risk foods. High risk foods are known to be more difficult to swallow and are more likely to cause coughing and choking. They should not be given to anyone on a modified diet.
Cognition
Following a stroke, you may find you struggle more to understand, organise, and interpret information. This can mean that you lose attention quickly or that you struggle to manage risks, plan activities and problem solve.
For further information, please visit the websites below:
Apps
Elevate – Brain Training Games. Elevate is an app that works on skills like memory, comprehension and processing. The app allows you to gradually progress the difficulty as you improve.
Lumosity. Lumosity is an app designed for adults of all ages. It has personalised challenges and games for memory, problem-solving and reasoning.
Vision
A stroke may affect your eyesight in several ways. It can cause missing areas in your visual field, problems with eye movements, visual processing problems and sensitivity to light. Depending on the way your eyes have been affected, you might be offered different treatment options.
An ophthalmologist is a professional who specialised in diagnosing and treating conditions that affect the eye. If you have noticed changes in your vision, it is important to contact your GP to request a referral for further assessment. If changes in your vision were noted while you were in hospital, it is likely they will have already completed a referral.
For further information on vision after stroke, visit: https://www.stroke.org.uk/stroke/effects/physical/vision-problems-after-stroke
Visual Inattention/ Neglect
Visual Inattention/Neglect is a common condition that occurs following a stroke. The person affected is not aware or ignores things on the affected side. They may hear you on the affected side, but they are not able to look at you.
It can result in the person only eating one half of the food on their plate or missing half of the page when they are reading.
It is important to be aware that they might not see you if you approach them on their affected side.
If you are supporting someone with their rehabilitation who has visual inattention, you may be asked to place objects and approach them on their affected side. They are likely to need encouragement to turn their head, to look and maintain their focus to this side.
However, if this condition is more severe, you might be advised to adjust the position of objects to allow them to compensate and use the unaffected side.
Apps
There are various apps and devices that can support you if you have a visual impairment.
VoiceOver: This app is a screen reader that reads text out loud on Apple Macs, iPads and iPhones.
Narrator: This app is a screen reader that reads text out loud on for computers or smartphones that use Microsoft Windows
Seeing AI: A free app for Apple devices that can recognise faces, objects, words and barcodes
Talking Goggles: The app can understand any image or word in seconds and then says what it sees.
Be My Eyes: This app links you with a sighted volunteer. For example, it uses the camera on your device so you can ask a volunteer something.
Evi: An app that you can ask questions by talking to it.
KNFB Reader: You can use it to read any words out loud or send them to a Braille display such as letters, menus and books.
AccessNote: An app that is a notetaker for Apple phones and tablets using VoiceOver.
Synapptic: A software for Android tablets and smartphones that can be used for emails, websites, photos and other things.
Guide Connect: A software for computers and TVs to access emails, websites and radio.
Fatigue
Fatigue is commonly experienced by stroke survivors and can affect your ability to do day-to-day activities or return to hobbies you previously enjoyed. Fatigue is often described as ‘a fatigue like no other’. It can be characterised as a disproportionate sense of tiredness, lack of energy and need to rest. However, rest may not improve it.
You may experience it early or later after a stroke. There are often multiple factors that contribute to the fatigue.
There are various ways to manage your fatigue. Your Occupational Therapist or Physiotherapist may have discussed some of these strategies with you previously. Find out more on this link.
For further information on fatigue after stroke and ways to manage it, see https://www.stroke.org.uk/resources/fatigue-after-stroke
There are various apps that can help you track your fatigue levels and prompt when you need to put strategies in place to manage it. You can search for these in your app store. Find out more here.
Posture and positioning
Why is good positioning important?
When you have a neurological condition, it can be harder to move and reposition yourself. If you spend time in a poor position, you might be at risk of problems such as:
- Pressure sores
- Chest infections
- Blood clots
- Urinary Tract Infections
- Constipation
- Reduced range of movement in joints (sometimes known as contractures)
- Blood pressure problems
- Swelling
- Stiffness and joint or muscle related pain
- Muscle spasticity
- Choking or coughing when you are eating
Good positioning can help prevent the problems outlined above and promote optimal recovery.
The optimal position for you will depend on the impact of your neurological condition on your movement, sensation and muscle tightness. If you are unable to reposition yourself, your caregiver might need to help you change position every few hours.
For example, after a stroke, you may lack sensation on one side of your body. This can make you feel unsafe when you are lying on this side. Careful positioning of pillows to support you can help to make you feel safer.
If you need specific support, you may be referred to wheelchair services for assessment of your needs. In Surrey wheelchairs are provided by Surrey Wheelchair services.
https://rosscare.co.uk/pages/surrey-wheelchair-service / surreywcs@rosscare.co.uk
Positioning leaflets:
Bed positioning for one sided weakness(hemiplegia)
Other Community resources
Stroke based community resources